BIO-MEDICAL WASTE MANAGEMENT
Introduction
Biomedical waste (BMW) is any waste produced during the diagnosis, treatment, or immunization of human or animal research activities pertaining thereto or in the production or testing of biological or in health camps. It follows the cradle to grave approach which is characterization, quantification, segregation, storage, transport, and treatment of BMW.
The basic principle of good BMW practice is based on the concept of 3Rs, namely, reduce, recycle, and reuse. The best BMW management methods aim at avoiding generation of waste or recovering as much as waste as possible, rather than disposing. Therefore, the various methods of BMW disposal, according to their desirability, are prevent, reduce, reuse, recycle, recover, treat, and lastly dispose. Hence, the waste should be tackled at source rather than “end of pipe approach.”
BMW treatment and disposal facility means any facility wherein treatment, disposal of BMW or processes incidental to such treatment and disposal is carried out.
Only about 10%–25% of BMW is hazardous, and the remaining 75%–95% is nonhazardous. The hazardous part of the waste presents physical, chemical, and/or microbiological risk to the general population and health-care workers associated with handling, treatment, and disposal of waste.
In a World Health Organization (WHO) meeting in Geneva, in June 2007, core principles for achieving safe and sustainable management of health-care waste were developed. It was stressed that through right investment of resources and complete commitment, the harmful effects of health-care waste to the people and environment can be reduced. All stakeholders associated with financing and supporting health-care activities are morally and legally obliged to ensure the safety of others and therefore should share in the cost of proper management of BMW. In addition, it is the duty of manufacturer to produce environment-friendly medical devices to ensure its safe disposal. WHO reinforced that government should designate a part of the budget for creation, support, and maintenance of efficient health-care waste management system. These include novel and ingenious methods/devices to reduce the bulk and toxicity of health-care waste. Nongovernmental Organization should undertake program and activities that contribute in this incentive.
Amendments in BMW rules
The first edition of WHO handbook on safe management of wastes from health-care activities known as “The Blue Book” came out in 1999. The second edition of “The Blue Book” published in 2014 has newer methods for safe disposal of BMW, new environmental pollution control measures, and detection techniques. In addition, new topics such as health-care waste management in emergencies, emerging pandemics, drug-resistant bacteria, and climate changes were covered in the second edition.
-430bbda1-9383-4a47-b4c3-3992d8f58497.png)
The new biomedical waste management rules have been notified to efficiently manage BMW in the country in 2016 These rules have been modified to include the word handling and bring more clarity in the application. In addition, strict rules have been made to ensure no pilferage of recyclables item, no secondary handling or in advent scattering or spillage by animals during transport from the Health care facility's to the common BMW treatment facility. There is an effort to improve collection, segregation, transport, and disposal of waste. Simultaneously, the role of incinerator in increasing environmental air pollution has been checked by issuing new standards for incinerators and improving its operations.
Benefits of the new biomedical waste rules as per 2016 guidelines
The new rules are stringent and elaborate and should bring about a change in the way, the BMW is being managed in India. Under the new rules, coverage has increased to include various health-care related camps such as vaccination camps, blood donation camps, and surgical camps.
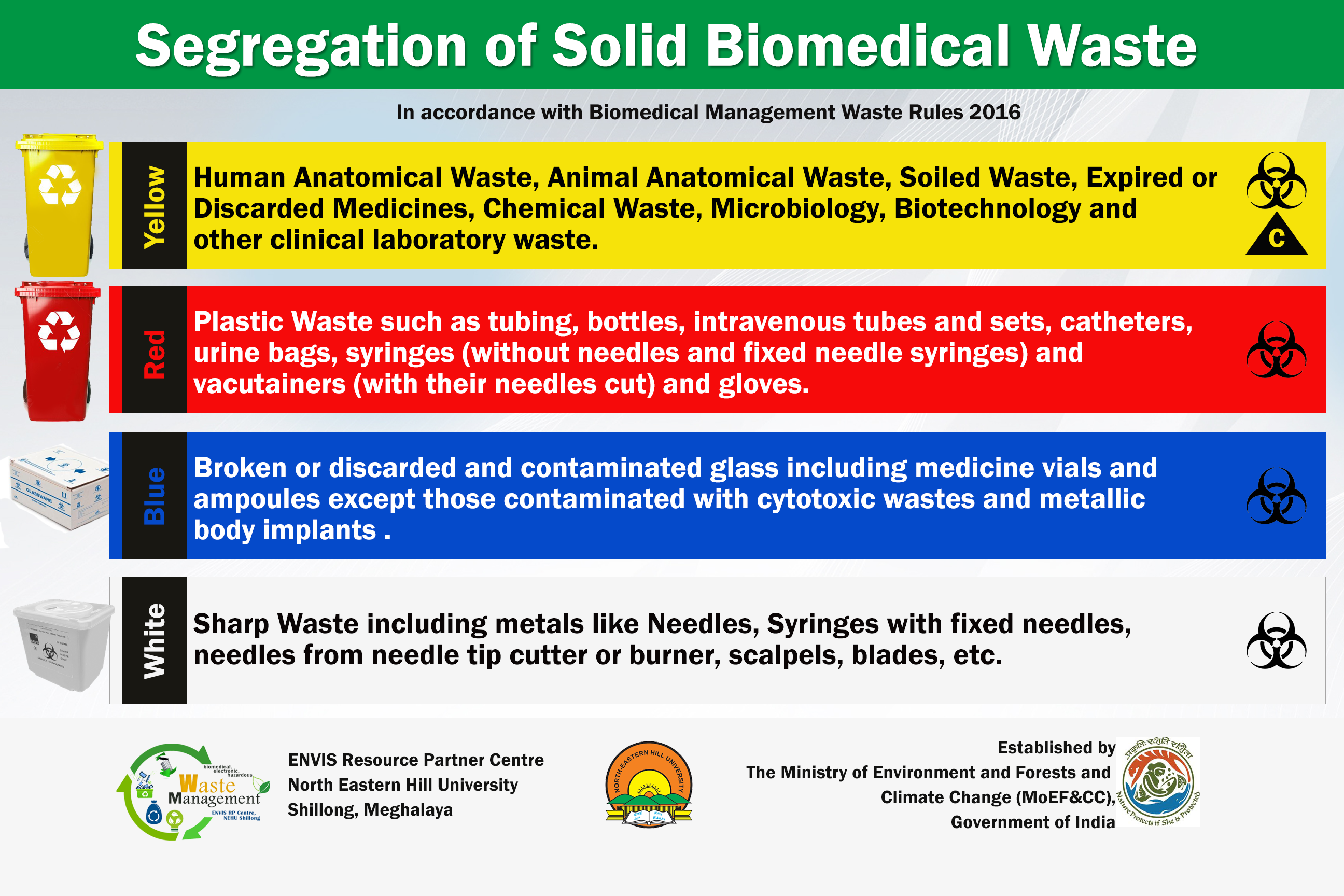
Another distinction is in the segregation, packaging, transport, and storage of BMW waste. The categories have been reduced to four to bring about ease of segregation. One of the main principle of disposal of BMW is that segregation has to be done at the source of generation of the waste. To overcome confusion created by large number of categories, this has been simplified to make it convenient and manageable for all HCWs. Now, the color coding (i.e., yellow, red, white, and blue) of the bags/containers is linked to a particular type of waste and its specific treatment option. For example, the disposal of chemical solid waste and cytotoxic waste to be done in yellow bag which goes for incineration/plasma pyrolysis/deep burial.
In addition, the health care fascility has to do pre-treatment of various laboratory waste and blood bags according to guidelines of WHO and NACO, to decrease chances of infections being transmitted to HCWs handling waste at treatment stage.
Within 2 years, plastic bags, gloves, and blood bags have to be phased out to eliminate emissions of dioxins and fur-ans during their burning into the environment. The new rule also calls for a bar code system for all bags/containers used for BMW treatment and disposal. This step will help in tracking and identifying bags during inspection for quality control and also quality assurance.
The BMW in red/blue bag or container which is for recycling will be sent only to an authorized recycler. This will keep the recycler in realm and in control of various government agencies. Greater emphasis has been given to recycling of waste to conserve resources as well as decrease pollution.
The 2016 guidelines are more specific regarding the dependence of health care facility on common biomedical waste treatment facility will provide land for setting up Common bio medical treatment facility State government or UT government will provide land for setting up Common bio-medical waste treatment facility. and no occupier of an Health care facility shall establish an on-site treatment and disposal facility if a Common bio-medical waste treatment facility is available within 75 kms.
This has several advantages as installation and functioning of individual BMW treatment facility as well as recruiting separate, dedicate, and skilled workforce require high capital investment. Common bio-medical waste treatment facility is a popular concept in developed countries because by operating it at its full potential, the cost of treatment/kg BMW gets significantly reduced. Further, this makes control and checking of various waste disposal plants less tedious. Furthermore, maintaining records and log book will streamline the documentation.
The emission standards for incinerator has been made more stringent (acceptable (S.P.M) Suspended Particulate Matter reduced to 50 mg/mm3, retention time in secondary camber lowered to 2 s). This will reduce dioxins and fur-ans release (which are produced at temperature greater than 600°C) and lead to production of carbon dioxide and water.
The new rules lays down new criteria for authorization of an health care facility and have made the procedure for getting authorization very simple. Bedded hospitals will get automatic authorization and non bedded Health care facility will get a one-time authorization.
Another improvement in the new rules is in the monitoring sector. The M.O.E.F (Ministry of Environment, Forest, and Climate change) will review health care facilities once a year through state health secretaries and the S.P.C.B (State Pollution Control Board). Moreover, according to the new rules, the advisory committee on BMW Management is now mandated to meet every 6 months.
Methods of disposal
Biological methods for disposal of BMW include an emerging system called “Bio-converter” 9 Biomedical Disposal, Inc.). It uses a solution of enzyme to decontaminate medical waste, and the resulting sludge is put through an extrudes used to remove water for sewage disposal and the solid waste is sent to landfill. Another method of environmental BMW disposal is the use of biodegradable plastics. Many biomedical implants built with biodegradable plastics undergo biological degradation with microbial extracellular enzymes. These microbes utilize these biodegradable polymers as substrate under starvation and in unavailability of suitable substrate. Further research needs to be done for large-scale economic manufacture of biodegradable plastics.
Segregation of Bio-medical waste
Treatment of Medical Waste
The primary methods of treatment and disposal of medical waste are:
Incineration
Autoclaves
Mechanical/Chemical Disinfection
Microwave
Irradiation
Vitrification
![Medical Waste Disposal – Definitive Guide 2020 [Infographic]](https://www.biomedicalwastesolutions.com/wp-content/uploads/2015/04/5-ways-of-treating-medical-waste.jpg)
The treated waste - if sufficiently sterile - can generally be disposed with waste in a sanitary landfill, or in some cases discharged into the sewer system. In the past, treatment of medical waste was primarily performed on-site at hospitals in dedicated medical waste facilities. Over time, the expense and regulation of these facilities have prompted organizations to hire contractors to collect, treat, and dispose of medical waste, and the percentage of medical organizations that perform their own treatment and disposal has dropped.

To ensure that the treatment method provides the proper environment for the destruction of microbes, test indicators for bacterial spores measure the treatment effectiveness.
Microbiological spores are among the most difficult of biological to destroy, so when the indicator package cannot be cultured after treatment, the waste is considered properly treated. In treatment methods where shredding or maceration is employed, the test package is inserted into the system after the shredding process to avoid physical destruction of the test package. The test package is then retrieved from the waste after treatment.
Incineration
Incineration is the controlled burning of the medical waste in a dedicated incinerator. Among industry professionals, these units are often referred to as hospital/medical/infectious waste incinerator.
Engineers often look at expected heat generated by combustion when choosing which incinerator to use: waste with heating value over 3500 kcal/kg is processed in a pyrolysis unit while lower heating value waste is burned in a single-chamber incinerator. Waste is typically heterogeneous, and if the combustible fraction is below 60 percent, it may not be acceptable for incineration. Overly wet waste (over 30 percent water by weight) is probably not good for incineration either as it will require excessive quantities of assist gas/fuel.
Incineration is an old technology and was widely used in the past for all sorts of waste. Individual buildings had their own waste incinerators in many cases. Incinerators got a bad reputation because of the air pollution they created and because the bottom ash, or clinker, was hard to keep under control. Members of the public unfortunately still have negative associations with incinerators. Today’s incineration units are typically much cleaner.
There are parts of the world where open pit burning still take place. And accidental fire - e.g. a house on fire - produce flames and smoke and debris. This makes “burning” and “combustion” bad words, but when approached from a cold hard engineering standpoint, incineration is often the best technology for treating medical waste. It can eliminate pathogens - even hard-to-kill bacterial spores - and can reduce the volume and mass of waste that goes to landfills considerably. Incineration can break down and render harmless hazardous organic chemicals. With proper technology, little acid gas is released to the atmosphere.
Incineration requires no Pre-treatment. Because most medical waste can be incinerated, the waste does not always require sorting or separation prior to treatment. Incineration has the benefit of reducing the volume of the waste by 80 percent or more, sterilizing the waste, and reducing the need for pre-processing the waste before treatment. The resulting incinerated waste can be disposed of in traditional methods, such as land filling. The downside of incineration is potential pollution from emissions generated during incineration. The EPA has stringent requirements on emissions from medical incinerators. The incineration process can be applied to almost all medical waste types, including pathological waste, and the process reduces the volume of the waste by up to 90%.
Modern incinerators incinerator can provide a secondary benefit by creating heat to power boilers in the facility.
The largest concern associated with incineration is air pollution from emissions. The EPA says that at least 20% of medical waste is plastic. Dioxins and fur-ans can be produced when these plastics burn. Old medical waste incinerators included no pollution control equipment but ones operating in the US today do.
Another concern is incinerator ash. As incinerators are designed or retrofitted with pollution prevention equipment, more of the potentially toxic chemicals that previously ended up in emissions now remain in the ash. The ash can be hazardous waste. Incinerator ash is generally disposed of in landfills after it is stabilized.
Downsides of incinerators
The public often has an aversion to incinerators and may raise objections if they hear one is being put in their area. The popular perception of incineration is informed by pictures of open pit burning done decades ago in the US and still today in some countries. Open pit burning is indeed not effective enough and results in smoke and other undesirable materials being released to the atmosphere. Most people don’t understand how incineration units can be made clean-burning and engineered to reduce the risk of dangerous releases. Most people also don’t understand how many incinerators are in their area already.
However, incineration can be a dirty process if not controlled adequately or if the process has not been designed correctly. Incineration can produce
Fine particles (in the smoke) - The particles can include heavy metals. If removed from the smoke before release, these particles are called fly ash and constitute another disposal problem.
Acid gases - these are formed during burning. Chlorine compounds, when burned, yield hydrochloric acid. Sulfur compounds yield sulfur dioxide or sulfur trioxide. Nitrogen oxides are produced in any high temperature treatment.
Ozone - indirectly. Nitrogen oxides from the exhaust can subsequently react with hydrocarbons in the air to produce ozone.
Bottom ash or sinter - the ashes after the incineration process is complete. Mostly inorganic material. This is disposed of in a landfill - either sanitary one or a hazardous waste one.
Heat - While good incinerators are insulated to save energy and protect workers, heat generation must be accounted for in facility and process design.
Even small incinerators can be optimized with good engineering design and operating procedures. The size and the throughput should be balanced to ensure a high residence time in the furnace. A good rule of thumb is to aim for 1200 degrees C with a vapor-phase residence time of 2 seconds.
Autoclave
Autoclaves can be used to process the large bulk of infectious waste produced at a hospital or clinic. Autoclaves come in a wide range of sizes and capacities. If you have steam in your facility, you can hook it up to a steam autoclave. Other autoclaves produce steam by electric heating.
Autoclaves medical waste is usually compacted after it cools down. The compaction process may include shredding before the compression. The compaction process reduces the volume of the treated waste significantly.
One problem with autoclaves is that the process can aerosol chemicals present in the waste, leading to the potential for release of materials you would prefer to not release. This can pose a hazard to human operators and to some extent the environment – even though the facility Heating, ventilation, and air conditioning (H.V.A.C) system may take much of the brunt. It is possible this aerosolized material will deposit on surfaces in duct-work or counter-tops and floors in health care facility.
Conclusion
Although these experts are in consensus that land filling waste is the most economical disposal method, they also agree that more recycling and resource reduction should be attained to reduce the continuous need for landfills.

Written By:
Priyanka Massey
Certified Infection Control Nurse & Professional Trainer
Ingenious Health Care Consultants Pvt.Ltd
Reference taken from Wikipedia.
Thanks for Your attention.