Promoting Hygiene To Minimize the Infections

Introduction
Healthcare Associated Infections (HCAI's) can occur following direct contact within healthcare settings or following surgery. These infections, the majority of which are preventable, can cause significant harm to those affected, increase hospital stay and put added pressure on the NHS.
There are many reasons a patient may develop a Health care associated infections, including weakened immune deference due to treatment for cancer or leukemia, complex surgical operations, insertion of medical devices such as catheters, or the over-use of antibiotics. The latter can result in the development of resistance such as meticillin-resistant Staphylococcus aureus (MRSA) making treatment with common antibiotics difficult. The increase in patients with chronic illnesses, such as diabetes, heart and kidney problems, and the increase in the elderly population are also contributing factors that predispose patients to infections.
Infection prevention and control measures, such as appropriate hand hygiene, environmental cleanliness, basic precautions during invasive procedures, and education of staff, patients and visitors, are simple and inexpensive measures to help reduce the risk of HCAI's.
How infections are spread/Mode of transmission
When healthcare staff are educated about the ways infections are spread it helps them to decide what preventative measures they need to take and they are better placed to inform patients. Spread of infection requires three elements. The first is an infectious agent - a bacteria, virus, fungi or protozoa. The source may be the patients’ own flora, other patients, staff or visitors, or contaminated equipment. The second element is a susceptible host –someone prone to infections because of an underlying disease, surgical procedures or indwelling devices, and the final factor is a means of transmission.
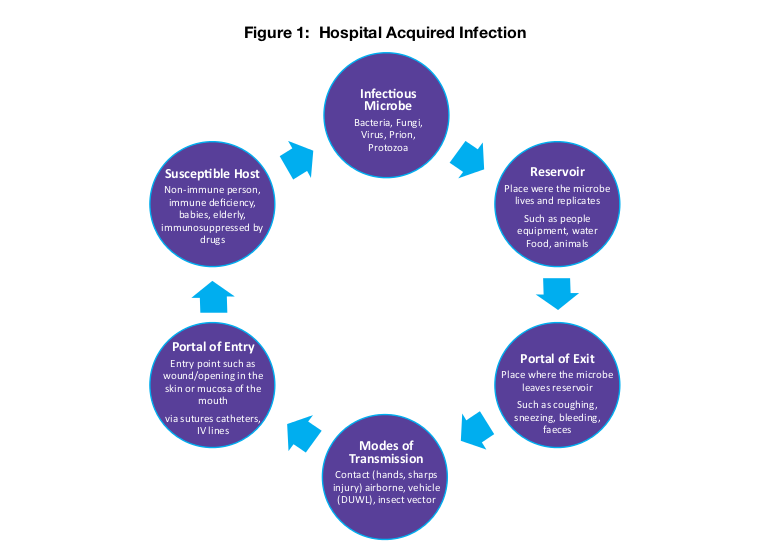
There are four main routes of infection transmission:
Contact transmission (direct or indirect):
Direct: body surface to body surface contact and physical transfer of microorganism between an infected or colonized (carrier) person to another or from one site to another in the same individual.
Indirect: contact between a person and contaminated surface or object.
Airborne /droplet transmission:
Droplet transmission: large droplets produced during coughing, sneezing, talking and suctioning generate droplets that land on surfaces which when touched can contaminate hands.
Airborne transmission: smaller micro-organisms, contaminated water particles or airborne dust particles containing the infectious agent are dispersed by air currents then inhaled or deposited onto horizontal surfaces, equipment etc.
Food and water (Fecal–oral) transmission:
Organisms can be transmitted via the food we eat and handle e.g. Campylobacter on raw chicken, by inappropriate handling of contaminated raw food or inadequate cooking. Cross-infection can occur via contaminated surfaces or infected food handlers if their hands are not cleaned after using the toilet. Water provides an ideal breeding ground for some micro- organisms, which can then be ingested, or as in Legionella inhaled.
Vector borne transmission:
These are infections transmitted by, flies, mosquitoes, and rats.
Hand hygiene
Hand hygiene is the single most important measure in reducing the risk of transmission of micro-organisms from one person to another or from one site to another on the same person. The World Health Organisation advises that cleaning hands promptly and as thoroughly as possible between patient contacts and after contact with blood, body fluids, secretions, excretions and contaminated equipment, is essential in order to minimize the risk of cross-infection in healthcare.

The Infection Prevention Society advises that effective hand hygiene involves the use of soap and water or alcohol hand rub. Liquid soap and warm running water can be used to mechanically remove transient micro-organisms from the hands and is perfectly acceptable for the vast majority of healthcare interventions. An alcohol-based product can be used for general hand hygiene in place of a hand-wash but only if hands are visibly clean. Alcohol rub, soap, water and paper towels must be available to encourage hand hygiene, and sinks for hand washing should be used for only that and not washing tea cups, dentures etc. A poster demonstrating the correct hand wash/rub techniques should be displayed at each clinical hand wash basin and a poster encouraging hand washing should be displayed in all patient and visitor toilets.
When building or refurbishing any health care environment provision of proper hand washing facilities must be a priority, therefore the Infection Prevention and Control Nurse (IPCN) should be involved at planning stage.
Environmental cleanliness in healthcare
Contaminated healthcare surfaces play a huge role in the transmission of dangerous pathogens, including Clostridium difficile and MRSA.

These pathogens are capable of prolonged survival on surfaces, therefore appropriate cleaning of those surfaces and equipment which patients and healthcare staff touch, is necessary to reduce transmission. Frequently touched surfaces, such as taps, door handles and light switches are more likely to harbor and transmit micro-organisms, so it’s important to ensure these surfaces are cleaned frequently in line with specifications for cleanliness in the NHS.
Public perception is very important and if the environment in which patients or their relatives are cared for appears unclean, it can lead to the perception that care is equally bad.
What patients and visitors can do to help in preventing HCAI's
While it is commonly perceived that HCAI's are attributable to healthcare staff, it is worth remembering that patients and their visitors also contribute. There are some simple things that patients and visitors should be encouraged to do in the fight to prevent transmission of infections.
Patients can: wash hands after using the toilet and before meals; cover mouth and nose with tissue when sneezing or coughing, bin the tissue and wash hands; if socializing at another patient’s bed space, clean hands afterwards; ask staff if they have washed their hands and/or changed their gloves before doing your care; wash/shower daily using own toiletries; keep locker and table top tidy and free from clutter to help with cleaning; do not interfere with drips, drains or dressings; and report any concerns about cleanliness or care standard.
Additionally, visitors can: use the hand sanitizer when entering and leaving the hospital ward or department; not visit if you are unwell especially with colds/flu or stomach upsets; avoid bringing very young children to visit; no not bring in fresh flowers or plants; speak to staff before bringing food into the hospital; and report any concerns about cleanliness or patient care.
It is only by staff, patients and visitors working together to do their bit that we will win the fight to reduce HCAI's.
WHO Recommendations: -

Conclusion: - Good Hygiene Practices Reducing the Spread of Infections and Viruses. The most important way to reduce the spread of infections is hand washing - always wash regularly with soap Providing boxes of tissues and encourage their use.

Written By : -
Priyanka Massey
Certified Infection Control Nurse,
Professional Trainer
Ingenious Health Care Consultants Pvt.Ltd.
Thanks for the attention.
Reference taken from Wikipedia






-430bbda1-9383-4a47-b4c3-3992d8f58497.png)
![Medical Waste Disposal – Definitive Guide 2020 [Infographic]](https://www.biomedicalwastesolutions.com/wp-content/uploads/2015/04/5-ways-of-treating-medical-waste.jpg)